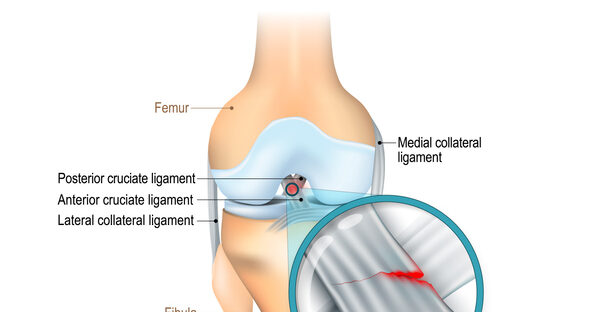
Tearing your ACL (anterior cruciate ligament) is one of the most challenging knee injuries especially if you’re active or play sports. Whether you’ve had surgery or are going the non-operative route, physiotherapy plays a vital role in your recovery. In this blog, we’ll walk you through the best physiotherapy exercises for ACL rehab, broken down by phase, to help you return to full function safely and confidently.
Why ACL Rehab Matters
The ACL is key to knee stability. Without proper rehab, you’re at risk of long-term weakness, instability, and re-injury. A structured physiotherapy plan strengthens the surrounding muscles, restores your range of motion, and improves coordination, especially important for athletes and active individuals.
Phase 1: Early Recovery (Weeks 1–3)
Goals: Reduce swelling, regain basic mobility, and activate key muscles.
Top Exercises:
- Heel Slides: Help restore range of motion without putting stress on the knee.
- Quad Sets: Gently wake up the quadriceps, which often shut down after injury.
- Straight Leg Raises: Build strength without bending the knee too much.
- Ankle Pumps: Improve circulation and reduce swelling.
Tip: Ice and elevation are your best friends during this phase.
Phase 2: Strength Building (Weeks 3–6)
Goals: Improve muscle strength, balance, and flexibility.
Top Exercises:
- Mini Squats (with support if needed): Activate glutes and quads in a controlled way.
- Bridges: Strengthen hamstrings, glutes, and core.
- Step-Ups: Use a small step to start re-training functional movement.
- Resistance Band Leg Presses: Provide controlled strengthening without joint impact.
Tip: Focus on slow, controlled movements and avoid compensating with your hips or back.
Phase 3: Functional Movement (Weeks 6–12)
Goals: Return to normal walking, jogging, and light sport-specific drills.
Top Exercises:
- Lunges (static and walking): Strengthen the entire lower limb chain.
- Balance Exercises on a Bosu Ball: Improve proprioception and stability.
- Side-Stepping with Band Resistance: Target the hip abductors for lateral support.
- Single-Leg Deadlifts: Rebuild strength, balance, and hamstring control.
Tip: Start incorporating light agility drills only under physiotherapist supervision.
Phase 4: Return to Sport (3–6+ Months)
Goals: Regain full strength, coordination, and confidence.
Top Exercises:
- Plyometric Drills (Jumping, bounding): Train explosive power and landing control.
- Agility Ladder Workouts: Build speed and reaction time.
- Sport-Specific Drills: Practice movements you’ll use in your sport.
- Single-Leg Hops: Test knee stability and readiness for dynamic activity.
When to See a Physiotherapist
Every ACL injury is different. Seeing a licensed physiotherapist ensures your rehab plan is safe, progressive, and tailored to your specific needs.
Rehabbing an ACL injury isn’t just about healing. It’s about coming back stronger, smarter, and more resilient. These physiotherapy exercises are essential building blocks, but consistent guidance and proper technique make all the difference. Stick with the process, trust your physio, and you’ll be back on your feet in no time. If you have injured your ACL and are looking to start physiotherapy, contact the professionals at Durham Orthopedic Clinic.