If you’re dealing with knee pain, your first thought might be that the joint itself is damaged.
But in many cases, knee pain isn’t only about the knee.
Tight muscles in the quadriceps, hamstrings, calves, or IT band can increase stress on the joint and change how it moves. When surrounding tissues become tight or overworked, discomfort often follows.
Massage therapy can play an important role in reducing that tension and supporting recovery.
How Massage Therapy Can Reduce Knee Pain
Massage therapy may help by:
- Reducing muscle tightness around the knee
- Improving circulation to irritated tissues
- Decreasing stiffness
- Supporting recovery after workouts
- Helping manage flare-ups
For many patients, knee pain improves when muscle tension is addressed alongside strengthening.
When Massage Is Most Helpful
Massage therapy is especially useful when knee pain is linked to:
- Tight quadriceps
- IT band irritation
- Calf tightness
- Overuse from sports or gym training
- Muscle soreness after increased activity
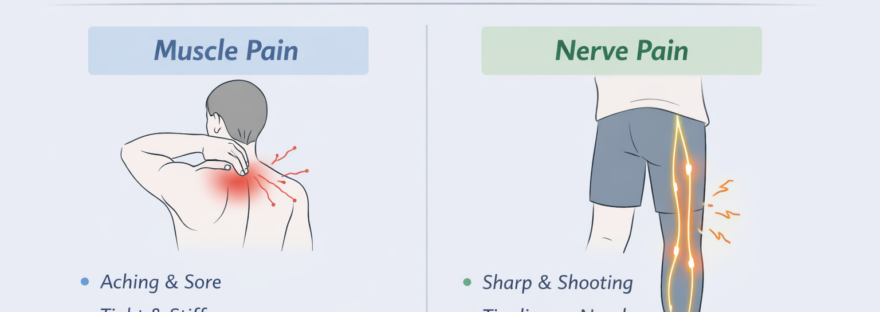
If your knee feels stiff, tight, or achy rather than unstable or severely swollen, massage may provide meaningful relief.
When Massage Alone May Not Be Enough
Massage therapy is excellent for soft tissue tension, but it doesn’t correct underlying weakness or joint mechanics.
These may include such issues as:
- Arthritis
- Meniscus irritation
- Ligament instability
- Poor hip or ankle mechanics
Massage vs Physiotherapy for Knee Pain
Massage focuses on:
- Muscle relaxation
- Circulation
- Soft tissue release
Physiotherapy focuses on:
- Strengthening
- Joint mechanics
- Movement retraining
- Long-term correction
What to Expect During a Massage for Knee Pain
Your Registered Massage Therapist may assess:
- Quadriceps tension
- Hamstrings
- Calf muscles
- IT band
- Hip mobility
Treatment typically avoids direct pressure on inflamed joints and instead focuses on surrounding tissues. After treatment, mild soreness is normal, but you should feel improved mobility and reduced tightness.
At-Home Tips to Support Knee Relief
Stay active within pain limits
Stretch quads and calves gently
Strengthen glutes and the muscles of the hip joint
Ice after flare-ups
Avoid deep painful movements temporarily until the pain improve
Massage works best when paired with smart movement.
When Should You Seek an Assessment?
Book an appointment if:
- Pain lasts more than 2–3 weeks
- You notice swelling or instability
- Pain interferes with stairs or walking
- Knee discomfort keeps returning
Early care prevents chronic compensation patterns.
Massage Therapy for Knee Pain in Ajax
If knee pain is limiting your workouts, workday, or daily activities, massage therapy at Durham Orthopedic Clinic may help reduce muscle tension and support recovery.
Contact us today for an assessment to determine whether massage alone is appropriate or whether combining it with physiotherapy will provide better long-term results.
Staying active and pain-free is possible with the right plan.